October 2024 – Addison’s disease, also known as primary adrenal insufficiency, is a rare yet serious condition that occurs when the adrenal glands fail to produce sufficient levels of cortisol and aldosterone. This hormonal imbalance can have a profound effect on various bodily functions, and without timely diagnosis and treatment, the disease can become life-threatening.
Today, we explore the latest developments in Addison’s disease, looking into its causes, symptoms, diagnosis, treatment options, and emerging research.
What Is Addison’s Disease?
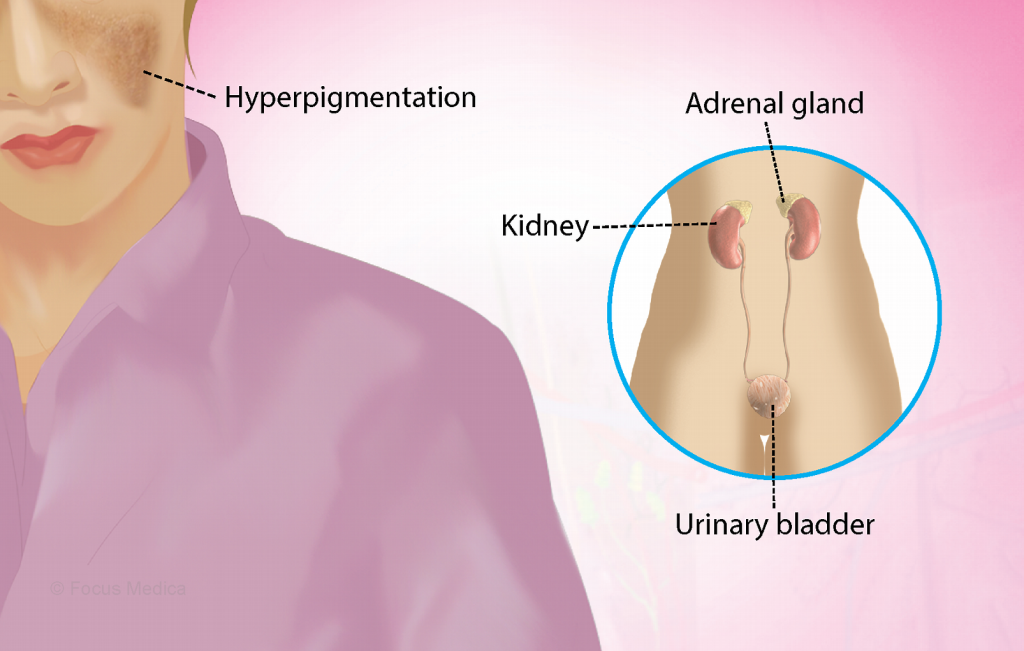
Addison’s disease is an endocrine disorder that disrupts the normal functioning of the adrenal glands. Located just above the kidneys, the adrenal glands are responsible for producing hormones essential to many of the body’s vital functions, particularly cortisol and aldosterone.
Cortisol, commonly referred to as the “stress hormone,” helps regulate blood sugar levels, metabolism, inflammation, and the body’s response to stress. Aldosterone, on the other hand, is critical for maintaining the balance of sodium and potassium in the body, which in turn influences blood pressure regulation. When these hormones are insufficient, a variety of symptoms can manifest, making daily life challenging and posing significant health risks.
Latest Insights Into Causes and Risk Factors
While the exact cause of Addison’s disease can vary, the majority of cases (approximately 70%) are due to autoimmune reactions. In these instances, the body’s immune system mistakenly attacks and damages the adrenal cortex, the outer layer of the adrenal glands, leading to hormone production failure.
Recent research has expanded our understanding of potential risk factors for developing Addison’s disease. Genetics play a key role; individuals with a family history of autoimmune conditions are at higher risk. New studies have also identified links between certain viral infections and the onset of Addison’s disease, suggesting that some pathogens may trigger autoimmune responses that damage the adrenal glands.
Additionally, Addison’s disease can result from infections such as tuberculosis (TB), which was historically a leading cause. Advances in healthcare have reduced TB-related cases, but the disease is still prevalent in areas where TB remains uncontrolled.
Other causes include adrenal gland tumors, bleeding into the adrenal glands, and certain medications that affect cortisol production.
Related Article: Addison’s Disease – Rare Endocrine Disorder and Recent Advances in Treatment
Symptoms of Addison’s Disease: What to Watch For
Addison’s disease symptoms develop gradually, making early diagnosis challenging. These symptoms often resemble those of more common health issues, such as chronic fatigue or depression, leading to frequent misdiagnosis.
Common symptoms of Addison’s disease include:
- Chronic fatigue: A persistent feeling of tiredness that does not improve with rest.
- Weight loss: Unexplained weight loss despite a normal diet.
- Low blood pressure: Particularly noticeable during sudden position changes (e.g., standing up).
- Salt cravings: A strong desire to consume salty foods, indicative of aldosterone deficiency.
- Muscle weakness: An inability to perform physical activities that were once manageable.
- Hyperpigmentation: Darkening of the skin, particularly on scars, joints, and pressure points.
- Gastrointestinal issues: Nausea, vomiting, diarrhea, or abdominal pain.
- Mood changes: Irritability, depression, or apathy.
In severe cases, individuals may experience an “Addisonian crisis,” a medical emergency where symptoms rapidly worsen, causing dehydration, low blood pressure, and a risk of shock or coma. Immediate medical attention is required in these situations.
The Importance of Early Diagnosis
Early diagnosis of Addison’s disease can prevent many of its severe complications. However, due to its rarity—affecting approximately 1 in 100,000 people—doctors may not always recognize the early signs.
Latest advances in diagnostic tools have improved the ability to identify Addison’s disease more accurately. Blood tests measuring cortisol, sodium, and potassium levels, alongside the ACTH stimulation test (a test that evaluates adrenal gland function), are key diagnostic methods. In some cases, imaging scans like CT or MRI are used to assess the condition of the adrenal glands.
Recent research has also pointed to advancements in genetic testing, which may soon allow for earlier detection in individuals with a family history of autoimmune diseases or endocrine disorders.
Treatment Options: Managing Addison’s Disease in 2024
Treatment for Addison’s disease focuses on replacing the hormones that the adrenal glands are no longer able to produce. This typically involves:
- Corticosteroid medications: Oral medications such as hydrocortisone, prednisone, or dexamethasone are prescribed to replace cortisol.
- Fludrocortisone: To replace aldosterone, patients may be given fludrocortisone to maintain the balance of sodium and potassium in the body.
Dosages may need to be adjusted during times of physical or emotional stress, as individuals with Addison’s disease are less able to respond to stress naturally. This makes stress management and lifestyle adjustments a critical part of the treatment plan.
Latest Innovations: Novel Treatments and Research
Exciting developments in Addison’s disease research are providing hope for better treatments and possibly even a cure. Scientists are exploring the potential of gene therapy to correct the genetic mutations responsible for autoimmune attacks on the adrenal glands.
Another area of interest is stem cell therapy. Researchers are investigating whether stem cells can be used to regenerate damaged adrenal tissue, potentially restoring hormone production and offering a more permanent solution than lifelong medication.
In addition, researchers are examining the role of immunosuppressive therapies to prevent the immune system from attacking the adrenal glands in autoimmune-related Addison’s disease cases. While still in the experimental stages, early results have been promising.
Patient Stories: Living with Addison’s Disease
The challenges of living with Addison’s disease can be profound, but many patients have found ways to lead full, active lives with proper treatment. One such individual is Jane Thompson, a 34-year-old who was diagnosed with Addison’s disease after experiencing extreme fatigue and unexplained weight loss for over a year.
“Getting a diagnosis was such a relief,” she says. “For so long, I felt like something was wrong, but I couldn’t pinpoint it. Once I started treatment, it was life-changing. The fatigue and weakness slowly started to improve, and I learned how to manage stress and take care of my body in new ways.”
Another patient, Mark Reyes, shared his story of navigating an Addisonian crisis, a severe medical emergency that can result from untreated Addison’s disease. “I collapsed at work and was rushed to the hospital. The doctors told me it was an Addisonian crisis—something I had never even heard of. It was terrifying. Now, I carry an emergency injection with me everywhere I go, just in case.”
These stories highlight the importance of awareness, early diagnosis, and individualized treatment plans.
Lifestyle Adjustments and Long-Term Management
Managing Addison’s disease is an ongoing process, but with the right tools and support, individuals can lead healthy lives. Key lifestyle adjustments include:
- Stress management: Because Addison’s disease affects the body’s ability to handle stress, patients must be proactive in managing emotional and physical stress. Meditation, yoga, and mindfulness practices are highly recommended.
- Diet: Maintaining a balanced diet rich in sodium is important for managing aldosterone deficiency. Some patients may need to increase their salt intake.
- Regular medical check-ups: Frequent consultations with endocrinologists are necessary to monitor hormone levels and adjust medications as needed.
One of the most important components of long-term management is educating patients on how to respond to emergencies. Those with Addison’s disease should always carry a medical alert bracelet and have access to emergency steroid injections to prevent or mitigate an Addisonian crisis.
Looking to the Future: Advancements in Addison’s Disease Research
As 2024 unfolds, the future of Addison’s disease research looks promising. With novel therapies like gene therapy, stem cell research, and immune system modulation under investigation, the potential for improved treatment outcomes has never been higher.
The medical community continues to work toward greater awareness and earlier detection of the disease, both of which are key to improving patient outcomes. In the meantime, support groups, patient advocacy organizations, and increased public awareness are playing an essential role in helping those affected by Addison’s disease to live better lives.
Conclusion
Addison’s disease remains a rare but serious condition with a profound impact on the lives of those affected. However, with early diagnosis, effective treatment, and ongoing medical advancements, many patients are able to manage their symptoms and lead full, active lives. As research continues to progress, the outlook for those living with Addison’s disease is brighter than ever.
Stay tuned for more updates as we track the latest developments in the treatment and management of this complex condition.

Dwayne Paschke specializes in writing, management, development, design and Search Engine Optimization. Although he has worked for 8 years in the industry, he never found an ideal person to work with as a partner. Later, he found Sebastian Pearson, and they both found specific understanding between them. Both of them divided their tasks in this project and are running this venture successfully.
